Byetta
Übersicht
Beschreibung
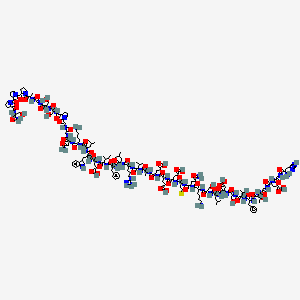
Exendin-4 is a peptide composed of 39 amino acids and is an analog of glucagon-like peptide-1 (GLP-1). It was originally isolated from the venom of the Gila monster lizard (Heloderma suspectum). Exendin-4 has garnered significant attention due to its insulinotropic properties, making it a valuable compound in the treatment of type 2 diabetes .
Vorbereitungsmethoden
Synthetic Routes and Reaction Conditions: Exendin-4 can be synthesized using recombinant DNA technology. One common method involves expressing the peptide in Pichia pastoris, a species of yeast. The gene encoding Exendin-4 is inserted into the yeast, which then produces the peptide. The peptide is subsequently purified using chromatography techniques .
Industrial Production Methods: For large-scale production, Exendin-4 is often produced using Escherichia coli or Pichia pastoris systems. The process involves the fermentation of these microorganisms, followed by purification steps to isolate the peptide. This method is cost-effective and suitable for mass production .
Analyse Chemischer Reaktionen
Arten von Reaktionen: Exendin-4 unterliegt verschiedenen chemischen Reaktionen, darunter:
Oxidation: Diese Reaktion kann an den Methioninresten innerhalb des Peptids stattfinden.
Reduktion: Disulfidbrücken innerhalb des Peptids können zu Thiolgruppen reduziert werden.
Substitution: Aminosäurereste innerhalb des Peptids können substituiert werden, um Analoga mit unterschiedlichen Eigenschaften zu erzeugen.
Häufige Reagenzien und Bedingungen:
Oxidation: Wasserstoffperoxid oder andere Oxidationsmittel.
Reduktion: Dithiothreitol (DTT) oder andere Reduktionsmittel.
Substitution: Site-directed Mutagenes-Techniken werden verwendet, um bestimmte Aminosäuren zu substituieren.
Hauptprodukte: Die Hauptprodukte, die aus diesen Reaktionen entstehen, umfassen oxidierte, reduzierte und substituierte Analoga von Exendin-4, die jeweils einzigartige Eigenschaften und potenzielle therapeutische Anwendungen besitzen .
Wissenschaftliche Forschungsanwendungen
Exendin-4 hat eine breite Palette von Anwendungen in der wissenschaftlichen Forschung, darunter:
Chemie: Wird als Modellpeptid für die Untersuchung von Proteinfaltung und -stabilität verwendet.
Biologie: Untersucht auf seine Rolle bei der Regulation des Glukosestoffwechsels und der Insulinsekretion.
Industrie: Eingesetzt bei der Entwicklung neuer therapeutischer Wirkstoffe für Stoffwechselstörungen.
5. Wirkmechanismus
Exendin-4 entfaltet seine Wirkung, indem es an den Rezeptor für Glucagon-like Peptide-1 (GLP-1R) bindet. Diese Bindung aktiviert die Adenylatcyclase, was zu einer Erhöhung des cAMP-Spiegels führt. Das erhöhte cAMP aktiviert die Proteinkinase A (PKA), die wiederum verschiedene Zielproteine phosphoryliert, die am Glukosestoffwechsel beteiligt sind. Diese Kaskade von Ereignissen führt zu einer verstärkten Insulinsekretion, einer reduzierten Glucagonsekretion und einer verbesserten Glukosehomöostase .
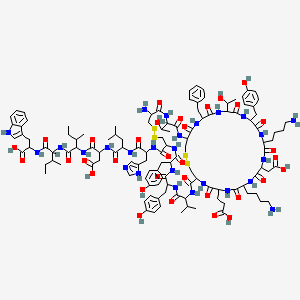
Ähnliche Verbindungen:
Glucagon-like Peptide-1 (GLP-1): Teilt strukturelle und funktionelle Ähnlichkeiten mit Exendin-4, hat aber eine kürzere Halbwertszeit.
Exenatid: Eine synthetische Form von Exendin-4, die klinisch zur Behandlung von Typ-2-Diabetes eingesetzt wird.
Einzigartigkeit: Exendin-4 ist aufgrund seiner längeren Halbwertszeit im Vergleich zu GLP-1 einzigartig, was es für die therapeutische Anwendung effektiver macht. Zusätzlich ist seine Herkunft aus dem Gift des Gila-Monsters ein faszinierender Aspekt seiner Entdeckung und Entwicklung .
Wirkmechanismus
Exendin-4 exerts its effects by binding to the glucagon-like peptide-1 receptor (GLP-1R). This binding activates adenylate cyclase, leading to an increase in cyclic adenosine monophosphate (cAMP) levels. The elevated cAMP activates protein kinase A (PKA), which in turn phosphorylates various target proteins involved in glucose metabolism. This cascade of events results in enhanced insulin secretion, reduced glucagon secretion, and improved glucose homeostasis .
Vergleich Mit ähnlichen Verbindungen
Glucagon-like peptide-1 (GLP-1): Shares structural and functional similarities with Exendin-4 but has a shorter half-life.
Exenatide: A synthetic form of Exendin-4 used clinically to treat type 2 diabetes.
Uniqueness: Exendin-4 is unique due to its longer half-life compared to GLP-1, making it more effective for therapeutic use. Additionally, its origin from the Gila monster’s venom adds a fascinating aspect to its discovery and development .
Eigenschaften
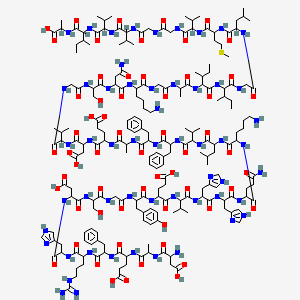
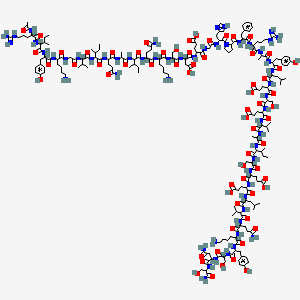
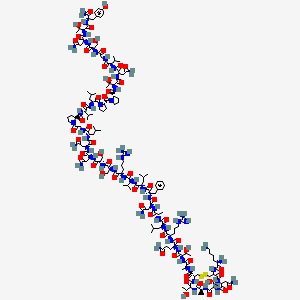
IUPAC Name |
5-[[2-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[6-amino-1-[[5-amino-1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[6-amino-1-[[4-amino-1-[[2-[[2-[2-[[1-[[1-[[2-[[1-[2-[2-[2-[(1-amino-3-hydroxy-1-oxopropan-2-yl)carbamoyl]pyrrolidine-1-carbonyl]pyrrolidine-1-carbonyl]pyrrolidin-1-yl]-1-oxopropan-2-yl]amino]-2-oxoethyl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]carbamoyl]pyrrolidin-1-yl]-2-oxoethyl]amino]-2-oxoethyl]amino]-1,4-dioxobutan-2-yl]amino]-1-oxohexan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-3-(1H-indol-3-yl)-1-oxopropan-2-yl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-3-methyl-1-oxopentan-2-yl]amino]-1-oxo-3-phenylpropan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-3-methyl-1-oxobutan-2-yl]amino]-1-oxopropan-2-yl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-4-methylsulfanyl-1-oxobutan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-1-oxohexan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-3-carboxy-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxobutan-2-yl]amino]-1-oxo-3-phenylpropan-2-yl]amino]-3-hydroxy-1-oxobutan-2-yl]amino]-2-oxoethyl]amino]-4-[[2-[[2-amino-3-(1H-imidazol-4-yl)propanoyl]amino]acetyl]amino]-5-oxopentanoic acid | |
|---|---|---|
| Details | Computed by Lexichem TK 2.7.0 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI |
InChI=1S/C184H282N50O60S/c1-16-94(10)147(178(289)213-114(52-58-144(257)258)163(274)218-121(73-101-77-195-105-39-24-23-38-103(101)105)168(279)215-116(68-90(2)3)165(276)205-107(41-26-28-61-186)158(269)219-122(75-134(189)243)154(265)198-79-135(244)196-83-139(248)231-63-30-43-129(231)175(286)225-127(87-238)174(285)223-125(85-236)155(266)200-80-136(245)202-96(12)181(292)233-65-32-45-131(233)183(294)234-66-33-46-132(234)182(293)232-64-31-44-130(232)176(287)222-124(84-235)150(190)261)229-170(281)119(71-99-34-19-17-20-35-99)217-166(277)117(69-91(4)5)214-159(270)108(42-29-62-194-184(191)192)212-177(288)146(93(8)9)228-151(262)95(11)203-156(267)111(49-55-141(251)252)208-161(272)112(50-56-142(253)254)209-162(273)113(51-57-143(255)256)210-164(275)115(59-67-295-15)211-160(271)110(47-53-133(188)242)207-157(268)106(40-25-27-60-185)206-172(283)126(86-237)224-167(278)118(70-92(6)7)216-169(280)123(76-145(259)260)220-173(284)128(88-239)226-180(291)149(98(14)241)230-171(282)120(72-100-36-21-18-22-37-100)221-179(290)148(97(13)240)227-138(247)82-199-153(264)109(48-54-140(249)250)204-137(246)81-197-152(263)104(187)74-102-78-193-89-201-102/h17-24,34-39,77-78,89-98,104,106-132,146-149,195,235-241H,16,25-33,40-76,79-88,185-187H2,1-15H3,(H2,188,242)(H2,189,243)(H2,190,261)(H,193,201)(H,196,244)(H,197,263)(H,198,265)(H,199,264)(H,200,266)(H,202,245)(H,203,267)(H,204,246)(H,205,276)(H,206,283)(H,207,268)(H,208,272)(H,209,273)(H,210,275)(H,211,271)(H,212,288)(H,213,289)(H,214,270)(H,215,279)(H,216,280)(H,217,277)(H,218,274)(H,219,269)(H,220,284)(H,221,290)(H,222,287)(H,223,285)(H,224,278)(H,225,286)(H,226,291)(H,227,247)(H,228,262)(H,229,281)(H,230,282)(H,249,250)(H,251,252)(H,253,254)(H,255,256)(H,257,258)(H,259,260)(H4,191,192,194) | |
| Details | Computed by InChI 1.0.6 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI Key |
HTQBXNHDCUEHJF-UHFFFAOYSA-N | |
| Details | Computed by InChI 1.0.6 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Canonical SMILES |
CCC(C)C(C(=O)NC(CCC(=O)O)C(=O)NC(CC1=CNC2=CC=CC=C21)C(=O)NC(CC(C)C)C(=O)NC(CCCCN)C(=O)NC(CC(=O)N)C(=O)NCC(=O)NCC(=O)N3CCCC3C(=O)NC(CO)C(=O)NC(CO)C(=O)NCC(=O)NC(C)C(=O)N4CCCC4C(=O)N5CCCC5C(=O)N6CCCC6C(=O)NC(CO)C(=O)N)NC(=O)C(CC7=CC=CC=C7)NC(=O)C(CC(C)C)NC(=O)C(CCCNC(=N)N)NC(=O)C(C(C)C)NC(=O)C(C)NC(=O)C(CCC(=O)O)NC(=O)C(CCC(=O)O)NC(=O)C(CCC(=O)O)NC(=O)C(CCSC)NC(=O)C(CCC(=O)N)NC(=O)C(CCCCN)NC(=O)C(CO)NC(=O)C(CC(C)C)NC(=O)C(CC(=O)O)NC(=O)C(CO)NC(=O)C(C(C)O)NC(=O)C(CC8=CC=CC=C8)NC(=O)C(C(C)O)NC(=O)CNC(=O)C(CCC(=O)O)NC(=O)CNC(=O)C(CC9=CNC=N9)N | |
| Details | Computed by OEChem 2.3.0 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Formula |
C184H282N50O60S | |
| Details | Computed by PubChem 2.1 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Weight |
4187 g/mol | |
| Details | Computed by PubChem 2.1 (PubChem release 2021.05.07) | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Mechanism of Action |
Islet amyloid, formed by aggregation of human islet amyloid polypeptide (hIAPP), is associated with beta cell death in type 2 diabetes as well as in cultured and transplanted human islets. Impaired prohIAPP processing due to beta cell dysfunction is implicated in hIAPP aggregation. We examined whether the glucagon-like peptide-1 receptor (GLP-1R) agonist exenatide can restore impaired prohIAPP processing and reduce hIAPP aggregation in cultured human islets and preserve beta cell function/mass during culture conditions used in clinical islet transplantation. METHODS: Isolated human islets (n = 10 donors) were cultured with or without exenatide in normal or elevated glucose for 2 or 7 days. Beta cell apoptosis, proliferation, mass, function, cJUN N-terminal kinase (JNK) and protein kinase B (PKB) activation and amyloid formation were assessed. ProhIAPP, its intermediates and mature hIAPP were detected. Exenatide-treated islets had markedly lower JNK and caspase-3 activation and beta cell apoptosis, resulting in higher beta/alpha cell ratio and beta cell area than non-treated cultured islets. Exenatide improved beta cell function, manifested as higher insulin response to glucose and insulin content, compared with non-treated cultured islets. Phospho-PKB immunoreactivity was detectable in exenatide-treated but not untreated cultured islets. Islet culture caused impaired prohIAPP processing with decreased mature hIAPP and increased NH(2)-terminally unprocessed prohIAPP levels resulting in higher release of immature hIAPP. Exenatide restored prohIAPP processing and reduced hIAPP aggregation in cultured islets. Exenatide treatment enhances survival and function of cultured human islets and restores impaired prohIAPP processing in normal and elevated glucose conditions thereby reducing hIAPP aggregation. GLP-1R agonists may preserve beta cells in conditions associated with islet amyloid formation., Incretins, such as glucagon-like peptide-1 (GLP-1), enhance glucose-dependent insulin secretion and exhibit other antihyperglycemic actions following their release into the circulation from the gut. Byetta is a GLP-1 receptor agonist that enhances glucose-dependent insulin secretion by the pancreatic beta-cell, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. The amino acid sequence of exenatide partially overlaps that of human GLP-1. Exenatide has been shown to bind and activate the human GLP-1 receptor in vitro. This leads to an increase in both glucose-dependent synthesis of insulin, and in vivo secretion of insulin from pancreatic beta cells, by mechanisms involving cyclic AMP and/or other intracellular signaling pathways., It has been reported that GLP-1 agonist exenatide (exendin-4) decreases blood pressure. The dose-dependent vasodilator effect of exendin-4 has previously been demonstrated, although the precise mechanism is not thoroughly described. /The aim of this study is/ to provide in vitro evidence for the hypothesis that exenatide may decrease central (aortic) blood pressure involving three gasotransmitters, namely nitric oxide (NO) carbon monoxide (CO), and hydrogen sulfide (H2S). ... The vasoactive effect of exenatide on isolated thoracic aortic rings of adult rats /was determined/. Two millimetre-long vessel segments were placed in a wire myograph and preincubated with inhibitors of the enzymes producing the three gasotransmitters, with inhibitors of reactive oxygen species formation, prostaglandin synthesis, inhibitors of protein kinases, potassium channels or with an inhibitor of the Na+/Ca2+-exchanger. Exenatide caused dose-dependent relaxation of rat thoracic aorta, which was evoked via the GLP-1 receptor and was mediated mainly by H2S but also by NO and CO. Prostaglandins and superoxide free radical also play a part in the relaxation. Inhibition of soluble guanylyl cyclase significantly diminished vasorelaxation. We found that ATP-sensitive-, voltage-gated- and calcium-activated large-conductance potassium channels are also involved in the vasodilation, but that seemingly the inhibition of the KCNQ-type voltage-gated potassium channels resulted in the most remarkable decrease in the rate of vasorelaxation. Inhibition of the Na+/Ca2+-exchanger abolished most of the vasodilation. Exenatide induces vasodilation in rat thoracic aorta with the contribution of all three gasotransmitters. /This provides/ in vitro evidence for the potential ability of exenatide to lower central (aortic) blood pressure, which could have relevant clinical importance., Glucagon-like peptide-1 receptor (GLP-1R) activation in the nucleus accumbens (NAc) core is pharmacologically and physiologically relevant for regulating palatable food intake. /An assessment was made/ whether GLP-1R signaling in the NAc core of rats modulates GABAergic medium spiny neurons (MSNs) through presynaptic-glutamatergic and/or presynaptic-dopaminergic signaling to control feeding. First, ex vivo fast-scan cyclic voltammetry showed that the GLP-1R agonist exendin-4 (Ex-4) does not alter dopamine release in the NAc core. Instead, support for a glutamatergic mechanism was provided by ex vivo electrophysiological analyses showing that Ex-4 activates presynaptic GLP-1Rs in the NAc core to increase the activity of MSNs via a glutamatergic, AMPA/kainate receptor-mediated mechanism, indicated by increased mEPSC frequency and decreased paired pulse ratio in core MSNs. Only a small, direct excitatory effect on MSNs by Ex-4 was observed, suggesting that the contribution of postsynaptic GLP-1R to MSN activity is minimal. The behavioral relevance of the electrophysiological data was confirmed by the finding that intracore injection of the AMPA/kainate receptor antagonist CNQX attenuated the ability of NAc core GLP-1R activation by Ex-4 microinjection to suppress food intake and body weight gain; in contrast, intracore NMDA receptor blockade by AP-5 did not inhibit the energy balance effects of NAc core Ex-4. Together, these data provide evidence for a novel glutamatergic, but not dopaminergic, mechanism by which NAc core GLP-1Rs promote negative energy balance. | |
| Details | PMID:24828651, Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4019807, Mietlicki-Baase EG et al; J Neurosci 34 (20): 6985-92 (2014) | |
| Record name | Exenatide | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/7789 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
Color/Form |
White to off-white powder | |
CAS No. |
141758-74-9 | |
| Record name | Exendin 3 (Heloderma horridum), 2-glycine-3-L-glutamic acid- | |
| Source | European Chemicals Agency (ECHA) | |
| URL | https://echa.europa.eu/information-on-chemicals | |
| Description | The European Chemicals Agency (ECHA) is an agency of the European Union which is the driving force among regulatory authorities in implementing the EU's groundbreaking chemicals legislation for the benefit of human health and the environment as well as for innovation and competitiveness. | |
| Explanation | Use of the information, documents and data from the ECHA website is subject to the terms and conditions of this Legal Notice, and subject to other binding limitations provided for under applicable law, the information, documents and data made available on the ECHA website may be reproduced, distributed and/or used, totally or in part, for non-commercial purposes provided that ECHA is acknowledged as the source: "Source: European Chemicals Agency, http://echa.europa.eu/". Such acknowledgement must be included in each copy of the material. ECHA permits and encourages organisations and individuals to create links to the ECHA website under the following cumulative conditions: Links can only be made to webpages that provide a link to the Legal Notice page. | |
| Record name | Exenatide | |
| Source | Hazardous Substances Data Bank (HSDB) | |
| URL | https://pubchem.ncbi.nlm.nih.gov/source/hsdb/7789 | |
| Description | The Hazardous Substances Data Bank (HSDB) is a toxicology database that focuses on the toxicology of potentially hazardous chemicals. It provides information on human exposure, industrial hygiene, emergency handling procedures, environmental fate, regulatory requirements, nanomaterials, and related areas. The information in HSDB has been assessed by a Scientific Review Panel. | |
Haftungsausschluss und Informationen zu In-Vitro-Forschungsprodukten
Bitte beachten Sie, dass alle Artikel und Produktinformationen, die auf BenchChem präsentiert werden, ausschließlich zu Informationszwecken bestimmt sind. Die auf BenchChem zum Kauf angebotenen Produkte sind speziell für In-vitro-Studien konzipiert, die außerhalb lebender Organismen durchgeführt werden. In-vitro-Studien, abgeleitet von dem lateinischen Begriff "in Glas", beinhalten Experimente, die in kontrollierten Laborumgebungen unter Verwendung von Zellen oder Geweben durchgeführt werden. Es ist wichtig zu beachten, dass diese Produkte nicht als Arzneimittel oder Medikamente eingestuft sind und keine Zulassung der FDA für die Vorbeugung, Behandlung oder Heilung von medizinischen Zuständen, Beschwerden oder Krankheiten erhalten haben. Wir müssen betonen, dass jede Form der körperlichen Einführung dieser Produkte in Menschen oder Tiere gesetzlich strikt untersagt ist. Es ist unerlässlich, sich an diese Richtlinien zu halten, um die Einhaltung rechtlicher und ethischer Standards in Forschung und Experiment zu gewährleisten.


![Benzeneacetic acid, alpha-[[(1,1-dimethylethoxy)carbonyl]amino]-4-methoxy-, (alphaR)-](/img/structure/B8064126.png)
![tert-butyl (5S)-2,4-dioxo-1,3,9-triazaspiro[4.5]decane-9-carboxylate](/img/structure/B8064146.png)
![(1'R,2R,3S,4'S,6S,8'R,10'Z,12'S,13'S,14'Z,16'Z,20'R,21'R,24'S)-2-cyclohexyl-21',24'-dihydroxy-12'-[(2R,4S,5S,6S)-5-[(2S,4S,5S,6S)-5-hydroxy-4-methoxy-6-methyloxan-2-yl]oxy-4-methoxy-6-methyloxan-2-yl]oxy-3,11',13',22'-tetramethylspiro[2,3-dihydropyran-6,6'-3,7,19-trioxatetracyclo[15.6.1.14,8.020,24]pentacosa-10,14,16,22-tetraene]-2'-one](/img/structure/B8064169.png)
![4-[[2-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[1-[[6-amino-1-[[5-amino-1-[[1-[[1-[[1-[[6-amino-1-[[6-amino-1-[[1-[[1-[[1-[[1-[[1-[[1-[[2-[[6-amino-1-[[1-[[1-[[6-amino-1-[[5-amino-1-[[1-[[1-[[6-amino-1-[[4-amino-1-[(1,6-diamino-1-oxohexan-2-yl)amino]-1,4-dioxobutan-2-yl]amino]-1-oxohexan-2-yl]amino]-3-methyl-1-oxobutan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-1-oxohexan-2-yl]amino]-3-(4-hydroxyphenyl)-1-oxopropan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-1-oxohexan-2-yl]amino]-2-oxoethyl]amino]-4-methyl-1-oxopentan-2-yl]amino]-3-methyl-1-oxobutan-2-yl]amino]-1-oxopropan-2-yl]amino]-1-oxopropan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-3-(4-hydroxyphenyl)-1-oxopropan-2-yl]amino]-1-oxohexan-2-yl]amino]-1-oxohexan-2-yl]amino]-3-methyl-1-oxobutan-2-yl]amino]-1-oxopropan-2-yl]amino]-4-methylsulfanyl-1-oxobutan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-1-oxohexan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-3-(4-hydroxyphenyl)-1-oxopropan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-(4-hydroxyphenyl)-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-carboxy-1-oxopropan-2-yl]amino]-3-hydroxy-1-oxobutan-2-yl]amino]-1-oxo-3-phenylpropan-2-yl]amino]-3-methyl-1-oxopentan-2-yl]amino]-2-oxoethyl]amino]-3-[[2-[[2-amino-3-(1H-imidazol-4-yl)propanoyl]amino]-3-hydroxypropanoyl]amino]-4-oxobutanoic acid](/img/structure/B8064182.png)
![4-[2-[[2-[[2-[[2-[[5-amino-2-[[2-[[5-amino-2-[[2-[[2-[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[1-[4-amino-2-[(2-amino-3-carboxypropanoyl)amino]-4-oxobutanoyl]pyrrolidine-2-carbonyl]amino]-3-hydroxypropanoyl]amino]-4-methylpentanoyl]amino]-3-hydroxypropanoyl]amino]-3-methylpentanoyl]amino]-3-carboxypropanoyl]amino]-4-methylpentanoyl]amino]-3-hydroxybutanoyl]amino]-3-phenylpropanoyl]amino]-3-(1H-imidazol-4-yl)propanoyl]amino]-4-methylpentanoyl]amino]-4-methylpentanoyl]amino]-5-carbamimidamidopentanoyl]amino]-3-hydroxybutanoyl]amino]-4-methylpentanoyl]amino]-4-methylpentanoyl]amino]-4-carboxybutanoyl]amino]-4-methylpentanoyl]amino]propanoylamino]-5-carbamimidamidopentanoyl]amino]-3-hydroxybutanoyl]amino]-5-oxopentanoyl]amino]-3-hydroxypropanoyl]amino]-5-oxopentanoyl]amino]-5-carbamimidamidopentanoyl]amino]-4-carboxybutanoyl]amino]-5-carbamimidamidopentanoyl]amino]propanoylamino]-5-[[5-amino-1-[[4-amino-1-[[1-[[1-[[1-[[1-[[1-[[1-[(1-amino-3-methyl-1-oxobutan-2-yl)amino]-3-hydroxy-1-oxopropan-2-yl]amino]-3-carboxy-1-oxopropan-2-yl]amino]-1-oxo-3-phenylpropan-2-yl]amino]-3-methyl-1-oxopentan-2-yl]amino]-3-methyl-1-oxopentan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-1,4-dioxobutan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-5-oxopentanoic acid](/img/structure/B8064199.png)
![5-[[5-amino-1-[[1-[[1-[[5-amino-1-[[18-[[4-amino-1-[[1-[[6-amino-1-[[1-[[1-[[1-[[1-[(1-amino-3-methyl-1-oxopentan-2-yl)amino]-3-methyl-1-oxopentan-2-yl]amino]-4-carboxy-1-oxobutan-2-yl]amino]-1-oxohexan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-1-oxohexan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-1,4-dioxobutan-2-yl]carbamoyl]-3-(1H-imidazol-4-ylmethyl)-6-methyl-2,5,8,12-tetraoxo-1,4,7,13-tetrazacyclooctadec-9-yl]amino]-1,5-dioxopentan-2-yl]amino]-1-oxopropan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-4-[2-[[2-[2-[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[[2-[(2-amino-3-phenylpropanoyl)amino]-3-(1H-imidazol-4-yl)propanoyl]amino]-4-methylpentanoyl]amino]-4-methylpentanoyl]amino]-5-carbamimidamidopentanoyl]amino]-4-carboxybutanoyl]amino]-3-methylbutanoyl]amino]-4-methylpentanoyl]amino]-4-carboxybutanoyl]amino]hexanoylamino]propanoylamino]-5-carbamimidamidopentanoyl]amino]propanoylamino]-5-oxopentanoic acid](/img/structure/B8064200.png)
![5-[[6-amino-1-[[5-amino-1-[[5-amino-1-[[1-[[1-[[4-amino-1-[[4-amino-1-[[1-[[1-[[1-[[1-[[1-[[1-[(1-amino-3-methyl-1-oxopentan-2-yl)amino]-3-hydroxy-1-oxobutan-2-yl]amino]-3-carboxy-1-oxopropan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-4-methyl-1-oxopentan-2-yl]amino]-5-carbamimidamido-1-oxopentan-2-yl]amino]-1,4-dioxobutan-2-yl]amino]-1,4-dioxobutan-2-yl]amino]-1-oxopropan-2-yl]amino]-1-oxopropan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-1,5-dioxopentan-2-yl]amino]-1-oxohexan-2-yl]amino]-4-[[6-amino-2-[[2-[[5-amino-2-[[6-amino-2-[[2-[[2-[[2-[[2-[2-[[6-amino-2-[[2-[[2-[[2-[[2-[(2-amino-3-phenylpropanoyl)amino]-3-(1H-imidazol-4-yl)propanoyl]amino]-4-methylpentanoyl]amino]-4-methylpentanoyl]amino]-5-carbamimidamidopentanoyl]amino]hexanoyl]amino]hexanoylamino]-3-methylpentanoyl]amino]-4-carboxybutanoyl]amino]-3-methylpentanoyl]amino]-4-carboxybutanoyl]amino]hexanoyl]amino]-5-oxopentanoyl]amino]-4-carboxybutanoyl]amino]hexanoyl]amino]-5-oxopentanoic acid](/img/structure/B8064214.png)
![(E,2S,4R,8S)-8-[(2S,5R,7S,8R,9R)-7-hydroxy-2-[(2R,4S,5S,7R,9S,10R)-2-[(2S,3S,5R,6R)-6-hydroxy-6-(hydroxymethyl)-3,5-dimethyloxan-2-yl]-9-[(2S,5S,6R)-5-methoxy-6-methyloxan-2-yl]oxy-4,10-dimethyl-1,6-dioxaspiro[4.5]decan-7-yl]-2,8-dimethyl-1,10-dioxaspiro[4.5]decan-9-yl]-2,4,6-trimethyl-5-oxonon-6-enoic acid](/img/structure/B8064229.png)
