Repaglinide
Vue d'ensemble
Description
Il appartient à la classe des méglitinides, des sécrétagogues d'insuline à action courte, qui agissent en se liant aux cellules β du pancréas pour stimuler la libération d'insuline . La répaglinide est connue pour son début d'action rapide et sa courte durée d'action, ce qui la rend efficace pour contrôler la glycémie postprandiale .
Applications De Recherche Scientifique
Repaglinide has several scientific research applications, including:
Chemistry: Used as a model compound for studying the synthesis and modification of antidiabetic drugs.
Biology: Studied for its effects on pancreatic β cells and insulin secretion.
Medicine: Used in clinical trials to evaluate its efficacy and safety in treating type 2 diabetes.
Industry: Employed in the development of new drug formulations and delivery systems to improve bioavailability and therapeutic outcomes
Mécanisme D'action
Target of Action
Repaglinide is an oral antihyperglycemic agent used for the treatment of non-insulin-dependent diabetes mellitus (NIDDM). It belongs to the meglitinide class of short-acting insulin secretagogues, which act by binding to β cells of the pancreas . The primary target of this compound is the ATP-sensitive potassium channels in the pancreatic beta cells .
Mode of Action
This compound lowers blood glucose levels by stimulating the release of insulin from the pancreas. This action is dependent upon functioning beta (β) cells in the pancreatic islets . It induces an early insulin response to meals, decreasing postprandial blood glucose levels . This compound increases insulin release by inhibiting ATP-sensitive potassium channels in a glucose-dependent manner .
Biochemical Pathways
This compound acts by blocking ATP-sensitive potassium channels in pancreatic beta cells, which in turn, stimulates insulin secretion . This mechanism of action involves promoting insulin release from β-islet cells of the pancreas . The influx of calcium ions stimulates calcium-dependent exocytosis of insulin granules .
Pharmacokinetics
This compound is extensively metabolized in the liver and excreted in bile . Approximately 90% of a single orally administered dose is eliminated in feces and 8% in urine . It has a bioavailability of 56% when taken orally and has a protein binding of over 98% . It is metabolized in the liver through oxidation and glucuronidation, mediated by CYP3A4 . The elimination half-life of this compound is about 1 hour .
Result of Action
The molecular effect of this compound involves the regulation of blood glucose levels by stimulating the release of insulin from the pancreas . On a cellular level, it acts by binding to β cells of the pancreas to stimulate insulin release . This results in a decrease in both postprandial and fasting blood glucose levels .
Action Environment
Environmental factors such as genetic polymorphisms can influence the efficacy of this compound. For instance, the IGF2BP2 rs1470579 and rs4402960 polymorphisms may affect the therapeutic efficacy of this compound in Chinese T2DM patients . Similarly, a variation in the KCNQ1 gene has been associated with the response to this compound . These genetic variations can influence the clinical expression of the drug and its effectiveness in controlling blood glucose levels.
Analyse Biochimique
Biochemical Properties
Repaglinide interacts with specific proteins in the body, particularly in the pancreas. It binds to ATP-sensitive potassium channels on the surface of pancreatic beta cells . This binding inhibits potassium efflux, leading to depolarization of the cell membrane and subsequent insulin release .
Cellular Effects
This compound has a profound effect on pancreatic beta cells. By stimulating insulin release, it helps regulate blood glucose levels. It also influences cell signaling pathways related to insulin secretion .
Molecular Mechanism
The molecular mechanism of this compound involves its binding to ATP-sensitive potassium channels on pancreatic beta cells . This binding inhibits the efflux of potassium ions, causing the cell to depolarize. This depolarization triggers the opening of calcium channels, leading to an influx of calcium ions, which then stimulate the release of insulin .
Temporal Effects in Laboratory Settings
In laboratory settings, the effects of this compound are observed over time. It has been found to have a sustained release, ensuring safety and improving the efficacy of the drug . The drug’s stability and degradation over time are factors that are considered in its formulation .
Dosage Effects in Animal Models
The effects of this compound in animal models vary with dosage. Studies have shown that it effectively lowers blood glucose levels in a dose-dependent manner .
Metabolic Pathways
This compound is involved in metabolic pathways related to glucose regulation. It interacts with enzymes and cofactors in these pathways, influencing metabolic flux and metabolite levels .
Transport and Distribution
This compound is transported and distributed within cells and tissues via specific transporters . Its localization and accumulation within cells can influence its efficacy .
Subcellular Localization
The subcellular localization of this compound is primarily at the cell membrane of pancreatic beta cells, where it interacts with ATP-sensitive potassium channels . This localization is crucial for its function in stimulating insulin release .
Méthodes De Préparation
Voies de synthèse et conditions de réaction
La répaglinide peut être synthétisée par un processus en plusieurs étapes impliquant plusieurs intermédiaires clés. Une méthode courante implique les étapes suivantes :
Estérification : L'acide 3-hydroxyphénylacétique est estérifié pour former l'éthyl 3-hydroxyphénylacetate.
Formylation : L'ester est ensuite formylé pour produire l'éthyl 3-formyl-4-hydroxyphénylacetate.
Oxydation : Le groupe formyle est oxydé en acide carboxylique, ce qui donne l'éthyl 3-carboxy-4-hydroxyphénylacetate.
Éthérification : Le groupe hydroxyle est éthérifié pour former l'éthyl 3-carboxy-4-éthoxyphénylacetate.
Hydrolyse sélective : L'ester est hydrolysé sélectivement pour produire l'acide 3-carboxy-4-éthoxyphénylacétique, un intermédiaire clé dans la synthèse de la répaglinide.
Méthodes de production industrielle
La production industrielle de répaglinide implique l'optimisation des conditions de réaction pour maximiser le rendement et la pureté. Cela comprend le contrôle de la température de réaction, du temps, du solvant et des rapports de substrats . Le processus est conçu pour être évolutif et respectueux de l'environnement, avec un minimum d'impuretés.
Analyse Des Réactions Chimiques
Types de réactions
La répaglinide subit plusieurs types de réactions chimiques, notamment :
Oxydation : La répaglinide peut être oxydée pour former divers métabolites.
Réduction : Les réactions de réduction peuvent modifier les groupes fonctionnels de la molécule de répaglinide.
Substitution : Des réactions de substitution peuvent se produire à différentes positions sur le cycle aromatique et les chaînes latérales.
Réactifs et conditions courants
Les réactifs courants utilisés dans la synthèse et la modification de la répaglinide comprennent :
Agents oxydants : tels que le permanganate de potassium et le peroxyde d'hydrogène.
Agents réducteurs : tels que le borohydrure de sodium et l'hydrure de lithium et d'aluminium.
Réactifs de substitution : tels que les halogènes et les agents alkylants.
Principaux produits
Les principaux produits formés à partir de ces réactions comprennent divers métabolites et dérivés de la répaglinide, qui peuvent être caractérisés à l'aide de techniques telles que la spectroscopie FT-IR, RMN et UV-Vis .
Applications de la recherche scientifique
La répaglinide a plusieurs applications de recherche scientifique, notamment :
Chimie : Utilisé comme composé modèle pour étudier la synthèse et la modification des médicaments antidiabétiques.
Biologie : Étudié pour ses effets sur les cellules β pancréatiques et la sécrétion d'insuline.
Médecine : Utilisé dans les essais cliniques pour évaluer son efficacité et sa sécurité dans le traitement du diabète de type 2.
Industrie : Employé dans le développement de nouvelles formulations de médicaments et systèmes d'administration pour améliorer la biodisponibilité et les résultats thérapeutiques
Mécanisme d'action
La répaglinide exerce ses effets en se liant aux canaux potassiques sensibles à l'ATP sur les cellules β du pancréas. Cette liaison inhibe l'efflux d'ions potassium, ce qui entraîne la dépolarisation de la membrane cellulaire. La dépolarisation ouvre les canaux calciques dépendants du voltage, permettant aux ions calcium d'entrer dans la cellule. L'afflux d'ions calcium déclenche l'exocytose des granules d'insuline, ce qui entraîne une augmentation de la libération d'insuline . Ce mécanisme est dépendant du glucose, ce qui signifie que la libération d'insuline n'est stimulée qu'en présence de glucose, réduisant le risque d'hypoglycémie .
Comparaison Avec Des Composés Similaires
La répaglinide est souvent comparée à d'autres médicaments antidiabétiques, tels que :
Nateglinide : Un autre méglitinide ayant un mécanisme d'action similaire mais une durée d'effet plus courte.
Sulfonylurées : telles que la glibenclamide et la glimépiride, qui stimulent également la libération d'insuline mais ont une durée d'action plus longue et un risque plus élevé d'hypoglycémie.
Métformine : Une biguanide qui réduit la production hépatique de glucose et améliore la sensibilité à l'insuline, mais ne stimule pas la libération d'insuline
La répaglinide est unique en son genre par son début d'action rapide et sa courte durée d'action, ce qui la rend particulièrement efficace pour contrôler la glycémie postprandiale sans provoquer d'hypoglycémie prolongée .
Propriétés
IUPAC Name |
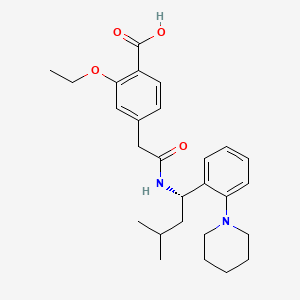
2-ethoxy-4-[2-[[(1S)-3-methyl-1-(2-piperidin-1-ylphenyl)butyl]amino]-2-oxoethyl]benzoic acid | |
|---|---|---|
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI |
InChI=1S/C27H36N2O4/c1-4-33-25-17-20(12-13-22(25)27(31)32)18-26(30)28-23(16-19(2)3)21-10-6-7-11-24(21)29-14-8-5-9-15-29/h6-7,10-13,17,19,23H,4-5,8-9,14-16,18H2,1-3H3,(H,28,30)(H,31,32)/t23-/m0/s1 | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
InChI Key |
FAEKWTJYAYMJKF-QHCPKHFHSA-N | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Canonical SMILES |
CCOC1=C(C=CC(=C1)CC(=O)NC(CC(C)C)C2=CC=CC=C2N3CCCCC3)C(=O)O | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Isomeric SMILES |
CCOC1=C(C=CC(=C1)CC(=O)N[C@@H](CC(C)C)C2=CC=CC=C2N3CCCCC3)C(=O)O | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Molecular Formula |
C27H36N2O4 | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
DSSTOX Substance ID |
DTXSID3023552 | |
| Record name | Repaglinide | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID3023552 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
Molecular Weight |
452.6 g/mol | |
| Source | PubChem | |
| URL | https://pubchem.ncbi.nlm.nih.gov | |
| Description | Data deposited in or computed by PubChem | |
Physical Description |
Solid | |
| Record name | Repaglinide | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0015048 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Solubility |
>67.9 [ug/mL] (The mean of the results at pH 7.4), 2.94e-03 g/L | |
| Record name | SID49648522 | |
| Source | Burnham Center for Chemical Genomics | |
| URL | https://pubchem.ncbi.nlm.nih.gov/bioassay/1996#section=Data-Table | |
| Description | Aqueous solubility in buffer at pH 7.4 | |
| Record name | Repaglinide | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0015048 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Mechanism of Action |
Repaglinide activity is dependent on the presence functioning β cells and glucose. In contrast to sulfonylurea insulin secretatogogues, repaglinide has no effect on insulin release in the absence of glucose. Rather, it potentiates the effect of extracellular glucose on ATP-sensitive potassium channel and has little effect on insulin levels between meals and overnight. As such, repaglinide is more effective at reducing postprandial blood glucose levels than fasting blood glucose levels and requires a longer duration of therapy (approximately one month) before decreases in fasting blood glucose are observed. The insulinotropic effects of repaglinide are highest at intermediate glucose levels (3 to 10 mmol/L) and it does not increase insulin release already stimulated by high glucose concentrations (greater than 15 mmol/L). Repaglinide appears to be selective for pancreatic β cells and does not appear to affect skeletal or cardiac muscle or thyroid tissue. | |
| Record name | Repaglinide | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00912 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
CAS No. |
135062-02-1 | |
| Record name | Repaglinide | |
| Source | CAS Common Chemistry | |
| URL | https://commonchemistry.cas.org/detail?cas_rn=135062-02-1 | |
| Description | CAS Common Chemistry is an open community resource for accessing chemical information. Nearly 500,000 chemical substances from CAS REGISTRY cover areas of community interest, including common and frequently regulated chemicals, and those relevant to high school and undergraduate chemistry classes. This chemical information, curated by our expert scientists, is provided in alignment with our mission as a division of the American Chemical Society. | |
| Explanation | The data from CAS Common Chemistry is provided under a CC-BY-NC 4.0 license, unless otherwise stated. | |
| Record name | Repaglinide [USAN:USP:INN:BAN] | |
| Source | ChemIDplus | |
| URL | https://pubchem.ncbi.nlm.nih.gov/substance/?source=chemidplus&sourceid=0135062021 | |
| Description | ChemIDplus is a free, web search system that provides access to the structure and nomenclature authority files used for the identification of chemical substances cited in National Library of Medicine (NLM) databases, including the TOXNET system. | |
| Record name | Repaglinide | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00912 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Repaglinide | |
| Source | DTP/NCI | |
| URL | https://dtp.cancer.gov/dtpstandard/servlet/dwindex?searchtype=NSC&outputformat=html&searchlist=759893 | |
| Description | The NCI Development Therapeutics Program (DTP) provides services and resources to the academic and private-sector research communities worldwide to facilitate the discovery and development of new cancer therapeutic agents. | |
| Explanation | Unless otherwise indicated, all text within NCI products is free of copyright and may be reused without our permission. Credit the National Cancer Institute as the source. | |
| Record name | Repaglinide | |
| Source | EPA DSSTox | |
| URL | https://comptox.epa.gov/dashboard/DTXSID3023552 | |
| Description | DSSTox provides a high quality public chemistry resource for supporting improved predictive toxicology. | |
| Record name | (+)-2-Ethoxy-alpha-(((S)-alpha-isobutyl-o-piperidinobenzyl)carbamoyl)-p-toluic acid | |
| Source | European Chemicals Agency (ECHA) | |
| URL | https://echa.europa.eu/information-on-chemicals | |
| Description | The European Chemicals Agency (ECHA) is an agency of the European Union which is the driving force among regulatory authorities in implementing the EU's groundbreaking chemicals legislation for the benefit of human health and the environment as well as for innovation and competitiveness. | |
| Explanation | Use of the information, documents and data from the ECHA website is subject to the terms and conditions of this Legal Notice, and subject to other binding limitations provided for under applicable law, the information, documents and data made available on the ECHA website may be reproduced, distributed and/or used, totally or in part, for non-commercial purposes provided that ECHA is acknowledged as the source: "Source: European Chemicals Agency, http://echa.europa.eu/". Such acknowledgement must be included in each copy of the material. ECHA permits and encourages organisations and individuals to create links to the ECHA website under the following cumulative conditions: Links can only be made to webpages that provide a link to the Legal Notice page. | |
| Record name | REPAGLINIDE | |
| Source | FDA Global Substance Registration System (GSRS) | |
| URL | https://gsrs.ncats.nih.gov/ginas/app/beta/substances/668Z8C33LU | |
| Description | The FDA Global Substance Registration System (GSRS) enables the efficient and accurate exchange of information on what substances are in regulated products. Instead of relying on names, which vary across regulatory domains, countries, and regions, the GSRS knowledge base makes it possible for substances to be defined by standardized, scientific descriptions. | |
| Explanation | Unless otherwise noted, the contents of the FDA website (www.fda.gov), both text and graphics, are not copyrighted. They are in the public domain and may be republished, reprinted and otherwise used freely by anyone without the need to obtain permission from FDA. Credit to the U.S. Food and Drug Administration as the source is appreciated but not required. | |
| Record name | Repaglinide | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0015048 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Melting Point |
130-131 °C, 130 - 131 °C | |
| Record name | Repaglinide | |
| Source | DrugBank | |
| URL | https://www.drugbank.ca/drugs/DB00912 | |
| Description | The DrugBank database is a unique bioinformatics and cheminformatics resource that combines detailed drug (i.e. chemical, pharmacological and pharmaceutical) data with comprehensive drug target (i.e. sequence, structure, and pathway) information. | |
| Explanation | Creative Common's Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/legalcode) | |
| Record name | Repaglinide | |
| Source | Human Metabolome Database (HMDB) | |
| URL | http://www.hmdb.ca/metabolites/HMDB0015048 | |
| Description | The Human Metabolome Database (HMDB) is a freely available electronic database containing detailed information about small molecule metabolites found in the human body. | |
| Explanation | HMDB is offered to the public as a freely available resource. Use and re-distribution of the data, in whole or in part, for commercial purposes requires explicit permission of the authors and explicit acknowledgment of the source material (HMDB) and the original publication (see the HMDB citing page). We ask that users who download significant portions of the database cite the HMDB paper in any resulting publications. | |
Synthesis routes and methods
Procedure details






Retrosynthesis Analysis
AI-Powered Synthesis Planning: Our tool employs the Template_relevance Pistachio, Template_relevance Bkms_metabolic, Template_relevance Pistachio_ringbreaker, Template_relevance Reaxys, Template_relevance Reaxys_biocatalysis model, leveraging a vast database of chemical reactions to predict feasible synthetic routes.
One-Step Synthesis Focus: Specifically designed for one-step synthesis, it provides concise and direct routes for your target compounds, streamlining the synthesis process.
Accurate Predictions: Utilizing the extensive PISTACHIO, BKMS_METABOLIC, PISTACHIO_RINGBREAKER, REAXYS, REAXYS_BIOCATALYSIS database, our tool offers high-accuracy predictions, reflecting the latest in chemical research and data.
Strategy Settings
| Precursor scoring | Relevance Heuristic |
|---|---|
| Min. plausibility | 0.01 |
| Model | Template_relevance |
| Template Set | Pistachio/Bkms_metabolic/Pistachio_ringbreaker/Reaxys/Reaxys_biocatalysis |
| Top-N result to add to graph | 6 |
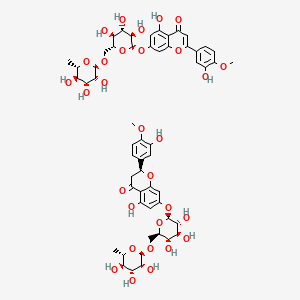
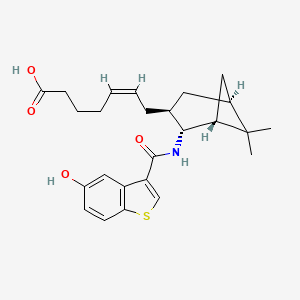
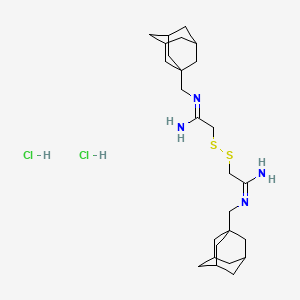
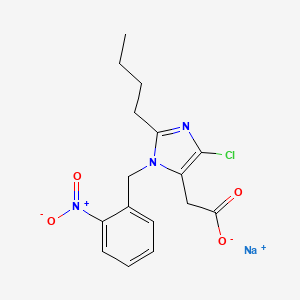
Feasible Synthetic Routes
Q1: What is the primary mechanism of action of repaglinide?
A: this compound is a non-sulfonylurea insulin secretagogue. It works by binding to and blocking ATP-sensitive potassium (K-ATP) channels on the surface of pancreatic beta cells. [, , , , ] This blockage depolarizes the beta cells, leading to the opening of voltage-gated calcium channels. The influx of calcium ions triggers the release of insulin from the beta cells. [, , , ]
Q2: How does the action of this compound differ from sulfonylureas?
A: While both this compound and sulfonylureas stimulate insulin release by binding to the sulfonylurea receptor 1 (SUR1) subunit of the K-ATP channel, they do so at distinct binding sites. [] This difference translates to a faster onset and shorter duration of action for this compound compared to sulfonylureas. [, , , , , ]
Q3: What is the impact of this compound on insulin secretion patterns?
A: this compound primarily amplifies the mass and amplitude of insulin secretory bursts without affecting the frequency of these bursts. [] This action enhances both early- and late-phase insulin secretion in response to hyperglycemia. []
Q4: What is the molecular formula and weight of this compound?
A: this compound has the molecular formula C27H36N2O4 and a molecular weight of 452.58 g/mol. []
Q5: Is there any spectroscopic data available for this compound?
A: Yes, this compound shows maximum UV absorbance at a wavelength of 237 nm in both phosphate buffer (pH 7.4) and 0.1 N HCl solutions. [] Fourier-transform infrared spectroscopy (FT-IR) analysis reveals characteristic peaks for this compound. [, ]
Q6: How does co-administration of this compound with cytochrome P450 (CYP)3A4 inhibitors affect its pharmacokinetics?
A: Strong CYP3A4 inhibitors, like ketoconazole, can increase the area under the curve (AUC) and peak plasma concentration (Cmax) of this compound, although to a lesser extent than expected due to its metabolism by multiple CYP enzymes. [] This interaction may necessitate adjustments in this compound dosage and blood glucose monitoring. []
Q7: Does the co-administration of this compound with CYP3A4 inducers impact its effectiveness?
A: Rifampicin, a potent CYP3A4 inducer, can significantly decrease the AUC and Cmax of this compound. [, , ] This interaction can potentially reduce the glucose-lowering effects of this compound, requiring dose adjustments and close monitoring. []
Q8: How does trimethoprim affect the pharmacokinetics and pharmacodynamics of this compound?
A: Trimethoprim, a CYP2C8 inhibitor, can significantly increase the plasma concentrations of this compound by inhibiting its CYP2C8-mediated metabolism. [, ] This interaction may increase the risk of hypoglycemia, particularly at higher doses. [, ]
Q9: Does grapefruit juice consumption impact the pharmacokinetics of this compound?
A: Grapefruit juice, a known inhibitor of intestinal CYP3A4, can increase the bioavailability of this compound, potentially leading to higher plasma concentrations. [] This effect is more prominent at lower doses of this compound. []
Q10: What is the absorption profile of this compound?
A: this compound is rapidly and completely absorbed from the gastrointestinal tract after oral administration. [, , ]
Q11: What is the time to peak plasma concentration (Tmax) for this compound?
A: Peak plasma levels (Cmax) are achieved within 1 hour (Tmax) of administration. [, ]
Q12: How is this compound metabolized and eliminated from the body?
A: this compound is primarily metabolized in the liver by CYP enzymes, mainly CYP2C8 and CYP3A4, into inactive metabolites. [, , , ] These metabolites are subsequently excreted primarily in bile. [, ]
Q13: Does the presence of the CYP2C8*3 allele affect the pharmacokinetics of this compound?
A: Contrary to some previous studies, research indicates that the CYP2C8*3 allele does not significantly alter the pharmacokinetics of this compound at therapeutic doses. []
Q14: Does the SLCO1B1 gene, which encodes for the OATP1B1 transporter, influence this compound disposition?
A: While pitavastatin, an OATP1B1 inhibitor, can increase this compound Cmax in individuals with specific SLCO1B1 genotypes, it does not significantly affect its overall pharmacokinetics or pharmacodynamics. [, ]
Q15: What is the primary therapeutic use of this compound?
A: this compound is primarily indicated for the treatment of type 2 diabetes mellitus, particularly in improving glycemic control. [, , , , , , ]
Q16: How does this compound compare to other antidiabetic agents in terms of efficacy?
A: In clinical trials, this compound demonstrated comparable efficacy to glibenclamide and gliclazide in improving glycemic control. [] It also showed superior efficacy to glipizide in maintaining glycemic control over a year. []
Q17: What is the role of this compound in combination therapy for type 2 diabetes?
A: this compound is often used in combination with other antidiabetic agents, such as metformin or thiazolidinediones, to enhance glycemic control. [, , , , , , ]
Q18: Can this compound be used as monotherapy in the treatment of type 2 diabetes?
A: Yes, clinical trials have shown this compound monotherapy to be effective in improving glycemic control in patients with type 2 diabetes. []
Q19: What formulation strategies have been explored to improve the solubility and dissolution rate of this compound?
A: Solid dispersions of this compound with polymers like polyethylene glycol (PEG), polyvinylpyrrolidone (PVP), mannitol, and urea have been investigated to enhance its solubility and dissolution rate. [, , , ]
Q20: Have any specific formulations, such as fast-dissolving tablets, been developed for this compound?
A: Yes, fast-dissolving tablets incorporating this compound solid dispersions and superdisintegrants have been developed to improve its bioavailability and potentially enhance its therapeutic efficacy. []
Q21: What is the rationale behind developing transdermal patches for this compound delivery?
A: Transdermal patches have been explored to achieve sustained release of this compound, improve patient compliance, and potentially reduce the frequency of administration. []
Q22: What are the most commonly reported adverse effects associated with this compound?
A: The most frequent adverse effects of this compound are hypoglycemia, upper respiratory tract infection, rhinitis, bronchitis, and headache. []
Q23: How does the risk of hypoglycemia with this compound compare to sulfonylureas?
A: Due to its shorter duration of action and meal-time dosing, this compound is associated with a lower risk of serious hypoglycemia compared to sulfonylureas, particularly if a meal is missed. [, , ]
Avertissement et informations sur les produits de recherche in vitro
Veuillez noter que tous les articles et informations sur les produits présentés sur BenchChem sont destinés uniquement à des fins informatives. Les produits disponibles à l'achat sur BenchChem sont spécifiquement conçus pour des études in vitro, qui sont réalisées en dehors des organismes vivants. Les études in vitro, dérivées du terme latin "in verre", impliquent des expériences réalisées dans des environnements de laboratoire contrôlés à l'aide de cellules ou de tissus. Il est important de noter que ces produits ne sont pas classés comme médicaments et n'ont pas reçu l'approbation de la FDA pour la prévention, le traitement ou la guérison de toute condition médicale, affection ou maladie. Nous devons souligner que toute forme d'introduction corporelle de ces produits chez les humains ou les animaux est strictement interdite par la loi. Il est essentiel de respecter ces directives pour assurer la conformité aux normes légales et éthiques en matière de recherche et d'expérimentation.
![Methyl 6-methyl-3-(2-methylpropyl)-4-(3-nitrophenyl)-4,7-dihydrothieno[2,3-b]pyridine-5-carboxylate](/img/structure/B1680436.png)
![methyl (4S)-6-methyl-3-(2-methylpropyl)-4-(3-nitrophenyl)-4,7-dihydrothieno[2,3-b]pyridine-5-carboxylate](/img/structure/B1680438.png)
![N-[4-methoxy-3-(4-methylpiperazin-1-yl)phenyl]-1,2-dihydrobenzo[e]indole-3-carboxamide;hydrochloride](/img/structure/B1680439.png)
![N-[4-[(3aR,9bS)-8-cyano-3,3a,4,9b-tetrahydro-1H-chromeno[3,4-c]pyrrol-2-yl]butyl]-4-phenylbenzamide](/img/structure/B1680441.png)
![tert-butyl 2-[[(3S)-2-[(2S)-2-[3-[(4-nitro-2,1,3-benzoxadiazol-7-yl)amino]propanoylamino]-3-phenylpropanoyl]-1,2-oxazolidine-3-carbonyl]amino]acetate](/img/structure/B1680447.png)
![3-Bromo-4-(4-(2-methoxyphenyl)piperazin-1-yl)-1H-pyrazolo[3,4-d]pyrimidine](/img/structure/B1680452.png)
![N-[(2S)-1-[[(2S)-2-[[(2S,3S)-1-cyclohexyl-3-hydroxy-6-pyridin-2-ylhexan-2-yl]amino]-3-(1H-imidazol-5-yl)propanoyl]amino]-1-oxo-3-phenylpropan-2-yl]-3-methylbutanamide](/img/structure/B1680457.png)
